Radiosurgery - Neolife Bucharest High Accuracy Stereotactic Radiosurgery Treatments
Stereotactic radiosurgery, also called radiosurgery, stereotaxis, similar to Gamma Knife, Cyber Knife treatments, is the radiotherapeutic treatment in which high doses of irradiation are administered with extremely high accuracy in the targeted tumour mass, reducing at the same time the dose received by the surrounding healthy tissues.
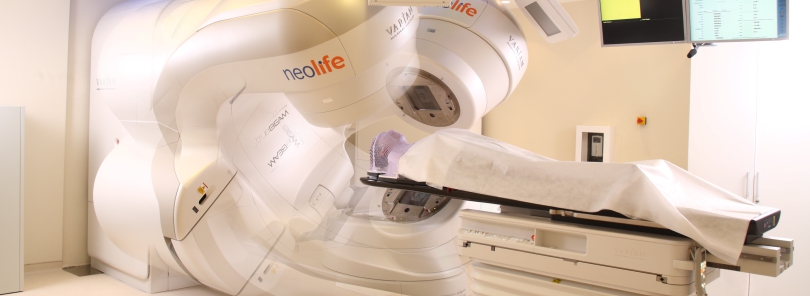
By using the TrueBeam system, in Neolife Medical Center in Bucharest, treatments of stereotactic radiosurgery can be performed at the highest standards and in compliance with the newest protocols in the field.
Since the opening of Neolife Medical Center, different patients have been treated with care and professionalism, with cerebral tumours, or tumours located in different regions, malignant or benign: meningiomas, gliomas (intracranial, intramedullary), glioblastomas, adenoid cystic carcinoma of the sphenoidal sinus, undifferentiated carcinomas of the rhinopharynx, ethmoid basal tumour masses, neurinomas, etc.
The treatments of stereotactic radiosurgery are non-invasive, unpainful, do not require anaesthesia, and the patients can leave the hospital, typically, on the same day of the procedure. Considering that it is a high-accuracy procedure, the patient's head must be immobilised. This immobilisation is performed in a non-invasive manner, by using a thermoformed fiber mask customised for each individual patient, unlike previous methods, that involved a stereotactic frame fixed on the cranium with four screws, a method that caused discomfort and even pain to some patients.
In addition, lesions that are not accessible to neurosurgery can be treated by radiosurgery.

Radiosurgery Techiques
Stereotactic radiosurgery (SRS)
view Stereotactic Body Radiation Therapy (SBRT)It applies for small brain tumours or other types of brain disorders, by delivering high doses of radiations with very high accuracy (accuracy below 1-2m).
Even though the name may suggest a surgical procedure, this method does not involve invasive treatments, and the name is given by the fact that this accurate technique of irradiation and release of a high dose of radiations in the tumour can result in the desired therapeutic outcome in only one or a few sessions. The term radiosurgery was coined by the Swedish neurosurgeon Lars Leksell from Karolinska Institute in order to describe the procedure used to administer high doses of irradiation in one session to a reduced intracranial volume.
Irradiation is performed either with multiple, non-coplanar beams, issued from different points, or by arc-therapy. The beams intersect at the level of the targeted mass, reducing the dose to the surrounding tissues.
The old stereotactic frame, that is still being used in gamma knife (stereotactic frame) represented the reference standard for SRS due to its following advantages:
However, there are some disadvantages related to the use of this device
Recent progress in the field of planning based on computer tomography (CT) and image guidance of RT have made it possible for new techniques to emerge, such those installed on TrueBeam, which no longer require the use of the stereotactic frame (frameless).
Potential advantages of replacing the invasive stereotactic frame include:
The irradiation is performed with :
CLINICAL USES OF SRS
Cerebral metastases
Cerebral metastases occur in 20-40% of cancer patients and represent the most frequent and commonly used indication for SRS.
Skull base meningiomas
SRS is an efficient non-invasive treatment for small meningiomas (< 3 cm in diameter). The local control rate is approximately 90% with reduced local toxicity (2.5-5%) for a follow-up monitoring period of 7 years.
Acoustic neuroma (vestibular schwannoma)
Local control after SRS for tumours with a diameter < 3 cm is de 92-98%, and local progression-free survival is 93%. (14, 15). Toxicity is reduced, with a risk of 1-5% for trigeminal or facial neuropathy, depending on the size of the tumour.
Hypophyseal adenomas
Approximately 10% of intracranial neoplasia occur in the hypophyseal region.
RT is in general reserved for patients with incompletely resected or relapsed tumours. Depending on the size and location of the treatment, conformational external RT or SRS can be used.
Local control with SRS is performed in >90% of cases for non-secreting tumours. If the patients are under hormonal suppression treatment, the results are poorer and can be explained by the underestimation of the real size of the tumour.
Stereotactic Body Radiation Therapy (SBRT)
view Stereotactic radiosurgery (SRS)Stereotactic Body Radiation Therapy – SBRT – is o non-invasive procedure, similar to SRS, the difference being that it applies for the treatment of tumours located outside the CNS (Central Nervous System)
SBRT uses:
High doses are administered for a shorter period of time as compared to conventional fractioned RT, while also reducing the exposure of normal tissues to high doses of irradiation
Clinical uses of SBRT:
NSCLC - Non-Small Cell Lung Cancer
Non-Small Cell Lung Cancer (NSCLC) - Lung cancer is the main cause of mortality caused by cancer worldwide. Most patients (75-85%) have NSCLC, and 15-25% are in stages 1 and 2
Vertebral metastases
Vertebral bone metastases occur relatively frequently in the evolution of malignant tumours. They are often symptomatic, accompanied by pain and neurologic deficit.
Conventional fractioned RT is a method of efficient palliative treatment for most patients. However, the capacity to administrate high doses, meant to control the tumour by this method, is limited by the tolerance of the bone marrow.
As a consequence, for patients that have tumour progression in a region that had been initially irradiated, surgery is required in order to avoid potential complications associated with repeated irradiation.
SBRT can represent a non-invasive alternative, providing adequate palliative effects, while also reducing the cumulated dose at the level of bone marrow. .
Hepatic metastases
Many patients are not eligible for invasive techniques (surgical resection, cryosurgery, injections with ethanol, ablation through radiofrequency). For such patients, SBRT can offer a non-invasive alternative, with similar benefits as those obtained in the treatment of single cerebral metastases.
view TrueBeam info